Learning to Unlearn: Observations from ESC and TCT 2022
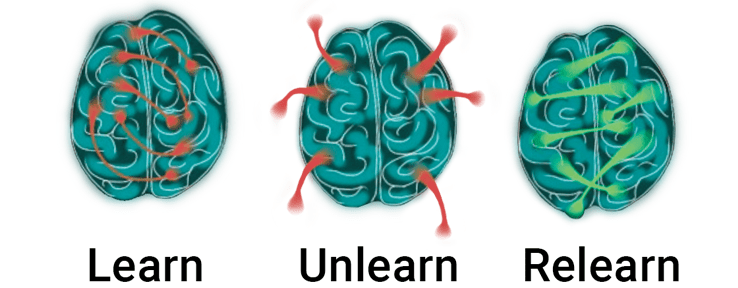
It is what we know already that often prevents us from learning.
– Claude Bernard
Over the past months, cardiologists around the world have had multiple opportunities to pause and consider if we need to unlearn certain beliefs that influence the way we care for our patients with coronary artery disease. During the recent European Society of Cardiology (ESC) and Transcatheter Cardiovascular Therapeutics (TCT) conferences, a substantial number of the clinical trial findings may have surprised many of us.
Potentially unexpected findings came from several arenas. Studies assessed the effectiveness of our clinical choices from our earliest interactions with asymptomatic people at risk for coronary artery disease (DANCAVAS) to how we approach ongoing follow-up after coronary revascularization (POST-PCI). In these studies and many others, we learned that common clinical decisions may need to be revisited and revised. Furthermore, the findings of the REVIVED trial seemed to upend what was learned from the STITCH trials in terms of how we should care for patients with left ventricular dysfunction and extensive coronary artery disease.
In contrast, other trials reinforced lessons we’ve learned before, such as the clinical utility of coronary physiology to guide clinical revascularization decisions. One such example, the FRAME-AMI trial, found that acute-MI patients did better when PCI of non-infarct related artery lesions was guided by invasive FFR rather than by visual angiography alone.
Perhaps most of all, the ADVANCE-DK findings seemed simultaneously to reinforce and disrupt prior learnings the most.
This 3-year follow-up of 900 patients from the ADVANCE registry demonstrated that information from a coronary CTA pathway with selective FFRCT, as highlighted in the 2021 ACC/AHA Chest Pain Guideline, enables clinicians to
- Identify Long-term Risk: Patients with abnormal FFRCT have significantly higher long-term risk of cardiovascular death or MI, regardless of calcium score.
- Improve Outcomes with FFRCT-Guided Revasc: Revascularization in vessels with abnormal FFRCT significantly reduces adverse cardiovascular events and improved patient QOL / satisfaction.
But wait… Didn’t the ISCHEMIA trial teach us that invasive management is no better than medical therapy in terms of reducing adverse events? How could this data claim to show that revascularization does anything beyond symptom alleviation?
Upon closer examination, ADVANCE-DK instructs us that the negative findings of ISCHEMIA may have far more to do with the tests that served as gatekeepers to the cath lab rather than the effectiveness of the treatments offered in that setting. By randomizing patients with abnormal stress tests but with no insight to coronary physiology such as FFR, ISCHEMIA certainly sent patients to ICA who had no reason to be there, while failing to identify patients for inclusion who had undiagnosed physiologically-significant coronary disease. The work of M. Sud, et al. explained most recently how this would disadvantage patients who are harmed by either revascularization in vessels with normal physiology or by failure to revascularize vessels with abnormal physiology.
As ADVANCE-DK makes clear, the information available via a coronary CTA-driven pathway with appropriate FFRCT provides clinicians with immediate insight into both the unique long-term cardiovascular risks a patient faces while also helping to guide appropriate treatment selection.
Now we must determine how we alter our work. Can we reassess prior lessons as new information elucidates what may have been previously misunderstood or not embraced? How will our patients benefit from what we unlearn?
— A perspective from HeartFlow Chief Medical Officer, Campbell Rogers, MD
Bio | LinkedIn





